By Akshay Patel, Senior Statistician at Exploristics
What is an estimand?
To facilitate clarity on precisely what a clinical trial intends to investigate, international trial regulatory guidelines (ICH E9(R1)) call for trialists to clearly define the treatment effects being investigated by using estimands. Following the ICH guidance, estimands are being recognised as a critical component of achieving patient-centricity in quality healthcare, which allows clear evaluation of treatments on patients’ lives. This will ensure trials provide the best evidence to define patient care.
An estimand is a precise statement of a research question and is the thing we want to estimate. Defining estimands is more than saying simply that we want to estimate the effect of a new treatment. Estimands also define who we count as having been successfully treated (what if people discontinue treatment?), and what population are we describing (if some people die before their outcomes are measured, we may find we are drawing conclusions on healthier people, who were able to survive the whole trial).
Why should we involve patients in discussions about estimands?
A key pain point for developers of new medicines is the recruitment and retention of clinical trial participants. This can be addressed to some extent by involving patients earlier in discussions around the planning of clinical trials. By bringing them in to the trial design process, patients feel that their input into clinical research is valued, and so are more likely to stay engaged in the clinical trials process.
Now with increasing attention being placed on using estimands in trial design, there is an opportunity to get patients involved in this critical part of trial design. This would be beneficial to many stakeholders. Not only could this encourage patient participation in clinical research, but it would also provide these patients with the direct benefit of evaluating treatments more clearly enabling them to make more informed decisions about their treatment choices. This in turn supports improve patient-centred outcomes and the evaluation of which treatments should be funded by healthcare systems and payers.
How can we support discussions on estimands?
While involving patients in defining estimands would benefit multiple stakeholders, what evidence is there that they would engage with this and how can it be facilitated in practice? As part of an NIHR Fellowship at Queen Mary University of London, I had the opportunity to work on a patient tool specifically designed to support the communication of estimands to public partners (i.e., patients and/or members of the public who are involved with or provide input to the research team) [1]. During this project, the team:
- co-developed a practical estimands explainer tool with public partners that describes what an estimands is and what impact it may have in trial results interpretation.
- explored public partners’ perspectives on the value of discussing estimands with them when designing a trial.
Developing a patient tool to explain estimands
Public partner interaction with the tool starts with being taken through an analogy of buying a new car and explains why individuals need to ask clear and specific questions about a car to understand whether it will perform as desired for them, as different individuals have diverse needs (Figure 1.). This example was used to illustrate how when testing a new treatment, all stakeholders need to be clear about the precise question being asked, so that the answer is meaningful and useful. The tool then takes users through further examples which demonstrate why this is important.
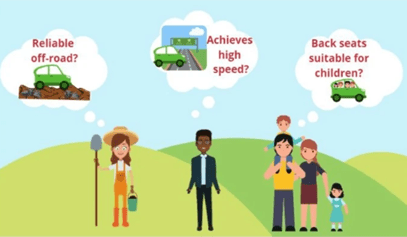
Figure 1. Asking the right questions to find the car you need, taken from Starting a conversation about estimands with public partners involved in clinical trials: a co-developed tool.
Feedback on the tool from the public partners was positive and indicated that they had found it useful to initiate a discussion about what question is being answered in a trial design context. This has provided a major step towards facilitating patient involvement in estimands discussions with the aim to rollout to larger groups and more diverse contexts.
Patient perspectives on improving engagement with clinical research
During the focus groups I led with public partners on this project, key insights on the interaction between clinical researchers and patients were raised. These included that:
- Research questions should be directly relevant to patients for example by selecting patient outcomes that matter. While they understood that many different questions could be answered using a clinical trial, they felt it was important to consider what questions a patient would want answered to increase engagement.
- An educational process is needed so that patients can be involved in the design, conduct, analysis and reporting of trials. To ensure that trials provide answers relevant to their participants, it was felt that there should be earlier involvement of public partners at initial trial planning meetings.
- Clear communication between patients and other stakeholders is required to ensure that the right questions are answered. Time should be invested in educating public partners in this unfamiliar area to support engagement.
- A change of culture is needed to facilitate greater engagement between public partners and clinical researchers. Public partners felt that there was a need to break down barriers in communication with researchers and that this couple be helped by avoiding technical jargon and using lay terms instead. When using more complex terms was unavoidable, it was felt that taking the time to explain these better could bridge the gap in understanding.
Education, communication and building trust
This project demonstrated that public partners are willing to get involved in discussing estimands but need clarity and educational support from researchers to do this. Previous studies on patient engagement in clinical trials [2,3] also highlight how communication issues and a lack of education on science and statistics creates a barrier to meaningful public engagement with clinical research. Moreover, a recent survey indicated that public partners felt current efforts to engage were tokenism [4]. To overcome this perception, there is a need to build trust through more proactive and practical efforts to engage with public partners that is responsive to their feedback. While this can be hard to deliver in a pressurised health system, it is still possible to make incremental steps to improve such outreach. The estimand explainer shows that this can be done. Shaped by public partner feedback, it provided a practical communication tool that was successful in supporting estimand discussions.
References:
- Cro, S., et al., Starting a conversation about estimands with public partners involved in clinical trials: a co-developed tool. Trials. 2023; 24: 443.
- Goulao, B., et al., Patient and public involvement in numerical aspects of trials (PoINT): exploring patient and public partner experiences and identifying stakeholder priorities. Trials. 2021; 22(1):499.
- Murray, E.J., et al., Patients and investigators prefer measures of absolute risk in subgroups for pragmatic randomized trials. J. Clin. Epidemiol. 2018; 103: 10-21.
- Minogue, V., et al., Patient and public involvement in reducing health and care research waste. Res. Involv. Engagem. 2018; 4(1):5.
Read more:
Estimands, the what and the how of drug discovery
Estimands, opportunity or risk for drug developers?
From cars to clinical trials, how simulation can improve design
Statistical Consulting Services
Watch more:
Matching trial objectives to design via the estimands framework




